About Hotze Health & Wellness Center
Since 1989, Hotze Health & Wellness Center has helped over 33,000 patients get their lives back using bioidentical hormones that restore hormones to optimal levels, strengthen immune systems, and increase energy levels. Our treatment regimen addresses the root cause of hypothyroidism, adrenal fatigue, menopause, perimenopause, low testosterone, allergies, and candida.
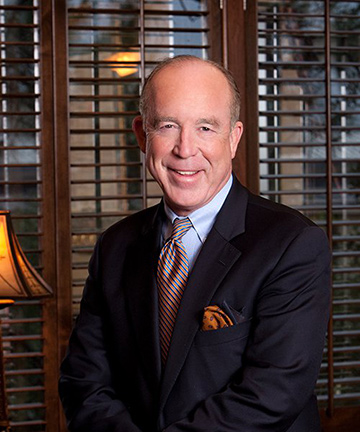
Led by best-selling author, radio host and leading natural health expert, Steven F. Hotze, M.D., our medical team has over 100 years’ combined medical experience backed by a staff of nearly 100 caring professionals who provide an environment of hope and extraordinary hospitality for each of our patients, who we call our guests. It is our deepest desire to help you obtain and maintain health and wellness naturally so that you may enjoy a better quality of life, pure and simple.
Click here to watch Dr. Hotze’s documentary as shown on the BIO channel.
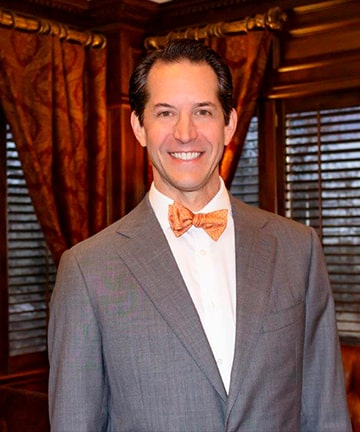
Meet Our Doctors
At Hotze Health & Wellness Center, our doctors are changing the way women and men are treated through the use of bioidentical hormones. Our natural treatments have helped over 33,000 individuals with hypothyroidism, adrenal fatigue, menopause, perimenopause, low testosterone, allergies, candida, detoxification and nutritional deficiencies.